“Practicing on patients” using a preceptor model is no longer accepted as safe or ethical practice in nursing education. Education done strictly in the clinical setting poses risks to patient safety and creates variation in educating to practice standards. Simulation in training, education, and professional development has been adopted as a safe venue to learn and practice clinical skills and decision making. Since 2013, Spectrum Health Grand Rapids (SHGR) offers the Simulation Center at the SHGR Cook Institute, providing 24,000 square feet of education and training space including 3,000 square feet of simulated hospital rooms for the use of simulation for nursing education and professional development.
The mission for the Simulation Center is to create safe, structured and effective learning environments using cutting edge techniques and technologies to engage health care providers in lifelike, relevant, hands-on experiences.
Course offerings in nursing education and professional development have grown and teaching modalities have shifted from didactic to hands-on practice. Clinical staff practice procedural skills and receive feedback on what they are doing well and what could be improved in a safe setting. All newly-hired clinical nurses come through classes spending portions of the day in self-learning stations and in-seat learning and then apply the knowledge they have gained in several simulations. Examples include caring for a patient with a tracheostomy and chest tube, a respiratory declining patient, and mock code scenarios where clinical nurses must quickly respond and escalate the chain of command. They take part in communication with other members of the clinical team to build collaboration skills. In the simulation program, participants are free to make mistakes, to ask questions, and to receive the support of a team around them.
The Simulation Center staff has built the inventory of procedural trainers, patient care manikins, and highly interactive simulators along with clinical equipment and supplies needed to support this authentic education. This equipment is shared through a user-friendly loan system both centrally in SHGR across many departments and to several Spectrum Health hospitals across the delivery system. Additionally, equipment is loaned to the cardiac cath lab, hyperbaric chamber, and disaster teams. As equipment is updated in the clinical setting across the delivery system, the sim program receives the identical equipment for education and training thus allowing the sim program to function without using clinical equipment needed for actual patient care.
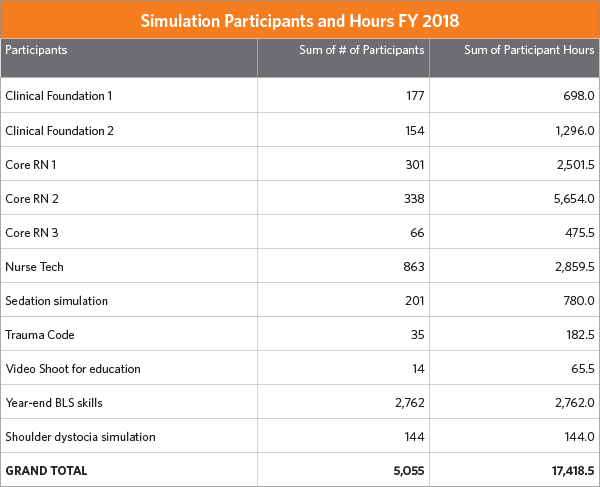
This year central classes with standard curriculum for nursing orientation and ongoing education and professional development include many simulation activities. This includes simulations for a new clinical foundations class, sedation, and onboarding nursing technicians. This standardized approach to curriculum design supports consistency and quality in education regardless of area of practice.
A major accomplishment of 2018 was the establishment of a perinatal safety program. Spectrum Health is the largest delivery hospital in the state of Michigan, with one of the largest Neonatal Intensive Care Units (NICU) in the country. Research indicates many perinatal crises are survivable, or even preventable. Nationally, simulation has been shown to improve performance and patient outcomes across patient populations. Simulation is particularly valuable for practicing infrequent, fast-paced situations that are tightly coupled with potential for severe patient harm. Obstetrical emergencies are infrequent yet demand high levels of skilled performance to be managed effectively. Clinical staff must perform fluidly in a demanding task that they rarely perform under the conditions of acute stress and high-stakes outcomes.
Leaders from the Simulation Center, in partnership with the Women and Infant Services (WIS) interprofessional leadership team, desired to create a comprehensive, unit-based simulation program focused on managing obstetrical emergencies for 300 staff, including clinical nurses, residents, mid-level and medical providers. This program was developed to reduce errors and provide better patient outcomes, reduce stress for clinical staff, improve communication and relationships (a culture of safety), and reduce medical-legal claims. SH was awarded a $100,000 grant to help start the program from the Hearst Foundation. Educators were trained at the Center for Advanced Pediatric and Perinatal Education (CAPE) at Stanford University, a national center for simulation, and the program was launched calendar year 2018. Lucina childbirth simulator and facilitator training, using grant support, helped launch the program.
To date 103 registered nurses and 41 providers have participated in the shoulder dystocia simulation. The simulations have also been integrated into the curriculum for new nurses and resident training. Thirty-one medical students have been able to use Lucina to simulate high-risk scenarios. Participation in the simulations has been well received by staff.
Another growing methodology supported at Cook is video production. The Spectrum Health InSite intranet platform supports video viewing. Video production has become a frequent request of our simulation services as nurse educators are using more self-learning and “flipping the classroom” techniques. A coordinator for simulation operations was hired this year with a background in simulation and video production and editing. This has allowed the ability to put “subtitles” on video for clinical nurses who view on the unit without sound. This has been an excellent methodology for pre-work to hands-on classes as well as providing “just-in-time” review for procedures that rapidly undergo change based on quality and safety data.
The simulation program through Spectrum Health Nursing offers a safe environment for learning, promoting both patient safety and positive patient outcomes. The simulation program has expanded this year to maintain up-to-date equipment in conjunction with what is used in practice, support simulation in departments outside of the Cook Institute, standardize new nurse onboarding experiences, enhance video capabilities, and support a large grant to offer simulation in the perinatal service line.