Improving the Specimen Identification Process
Specimen identification is a critical health care process that can have profound effects on patient outcomes when done incorrectly. In 2016, Spectrum Health Grand Rapids had 701 reported specimen identification (Specimen ID) errors out of 1,709,051 collections. This means an error rate of 410 errors per million collections at baseline. Specimen ID errors create risks to patient safety such as delays in care, increase cost, and may lead to wrong diagnosis, patient harm and even death. The Joint Commission’s National Patient Safety Goal number one is to “improve the accuracy of patient identification” which includes the use of two patient identifiers.
An Interdisciplinary Specimen Identification Committee was established in 2016 and best practices from Helen DeVos Children’s Hospital and Butterworth Emergency Departments were reviewed. The goal of the Specimen Identification Committee was to reduce Specimen ID errors caused by mislabeled and unlabeled specimens and to decrease the incidence of specimen labeling errors across the organization.
Initiatives implemented to reduce specimen ID errors included:
- In the moment error notification from lab to charge nurse and specimen collector via phone call
- Specimen ID error reporting at Daily Check In (DCI) to raise awareness across the organization
- Standard work for specimen collection and identification
- Standardized error follow up process
Despite these efforts the Specimen ID rates did not decrease and the committee identified a need for standard care flows that would reduce the incidence of unlabeled or mislabeled specimens. An Epic Care Flow (a visual diagram reflecting standard work) for all clinicians that collect specimens was developed to assure that all specimens are labeled correctly. The Care Flow applies to the collection of all specimens regardless of what type of device is being used to collect the specimen or where the printer for producing the specimen label is located. Communication of the Epic Care Flow for Specimen ID included committee members presenting information at NEXUS Clinical Readiness Days prior to Wave 1 and Wave 2 Go-Live. System wide education was also deployed to all nursing staff prior to Go-Live via the Spectrum Health Electronic Learning System (SHLI).
In November 2017, the new Epic Care Flow for Specimen ID was implemented with the EPIC EHR Wave 1 Go-Live. This included standard work as well as bar code scanning and in room printers for Intensive care units and the Emergency Department:
- Utilizing the available technology, the bar code scanning sequence assures that the patient wristband is scanned immediately prior to collecting the specimen and the specimen label is scanned after it is attached to the specimen. If bar code scanning is not available then two patient identifiers continues to be the process to assure patient safety standards.
- Printers previously were only available in shared spaces and staff had to sift through various patients to find the right label. To prepare for Epic Go-Live, printers were purchased and installed in every ICU room and every ED room. Staff are still expected to review printed labels to assure they are for the correct patient, in-room printers support correct specimen labeling.
Epic technology improves lab efficiency in that in most situations, all labs to be collected in a specimen container are combined to generate one label. Prior to Epic Go-Live, multiple labels were produced for each specimen and loose labels accompanied every collected specimen. With the new process, extra labels should prompt the staff member to double check that each specimen is labeled prior to sending to lab.
Outcomes:
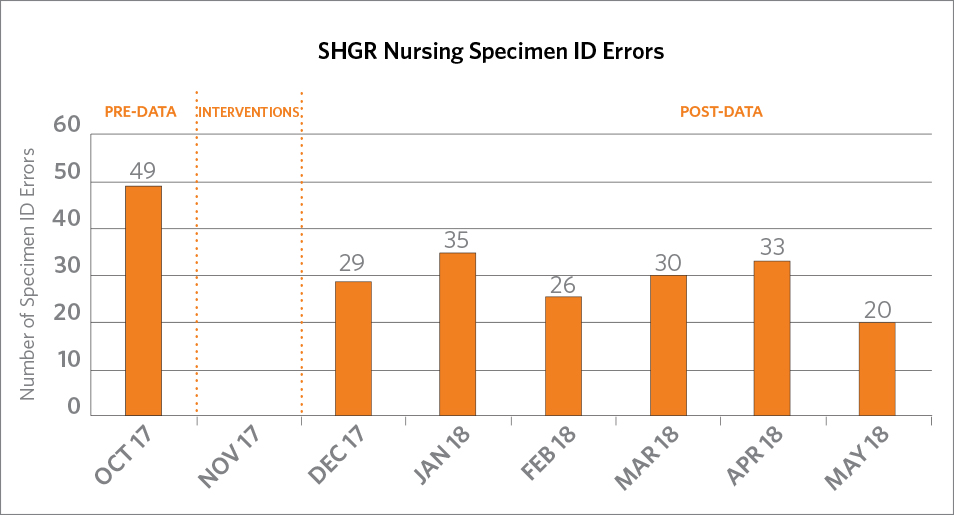
The number of Specimen ID errors in October 2017 was 49. Since EPIC Wave 1 Go-Live with its robust staff education, bar code scanning and additional printers placed in the intensive care units and Emergency Department, the number of Specimen ID errors decreased to 24 in November 2017 and 20 in May 2018.
Specimen Identification Committee Team
Beth Huizinga, MSN, RNC-NIC Clinical Nurse Specialist NICU
Luann Huizinga, BSN, RN, CPHQ Senior Quality Improvement Specialist
Jeff Skinner MHA, BSN, RN, CEN Nurse Manager Spectrum Health Butterworth Emergency Services
Colleen Tacoma DNP, RN, NE-BC, CMSRN Director of Adult Critical Care, Cardiothoracic & Cardiovascular Nursing
Sue Smith, MT (ASCP), MM, Senior Director Laboratory Services
Valerie Wassenar, Improvement Specialist, Laboratory
Jessika Carter, Clinical Informatics Specialist, Laboratory
Julie Nelson, Improvement Specialist, Laboratory
Yvonne Jackson, MSN, RN Clinical Informatics Specialist
Erika Makarewicz, Administrative Assistant, Laboratory
Joyce VanderMay, Supervisor, Laboratory
Milla Kreys, BSN, RN, CCRN, Clinical Nurse, Adult Critical Care CTICU
Jodi Swain MBA MSN RN CNML, Manager Clinical Operations and Improvement
