A3, MDI, and iHub are not medical terms, but they are part of the continuous quality improvement language that Spectrum Health has adopted to sharpen its focus on excellence. A critical aspect of continuous quality improvement is that the work aligns with system priorities. Spectrum Health has adopted new structures and processes to ensure this alignment through organizational deployment. These system priorities are now called “blue chips’. A blue chip simply identifies the most important goals to focus on as an organization to achieve our mission and vision. This process allows us to better understand our challenges and create an improvement strategy across the delivery system verses working in silos. Following an organizational deployment model also allows better connectivity from the work done at the unit or department level and how it supports the overall organizational goals.
A3 thinking is a methodology used as part of the LEAN process improvement model adopted by Spectrum Health as a management operating system. A cascading approach to setting goals is utilized and begins with creating strategic A3’s for each goal. These are then broken down into specific objectives for each goal, strategies for achieving the goal, and metrics to measure success. Each strategic goal is then transitioned into local process-level goals (hypotheses) that are monitored and reported weekly to senior leaders. Utilizing A3 thinking within the organizational deployment process allows for better understanding of the issues within the care process that need to be addressed and identification of specific countermeasures (interventions). Reporting and reviewing metrics weekly allows more real-time information as to whether the countermeasures (interventions) are delivering the expected outcome. If a specific countermeasure is not delivering the outcome expected, a review to identify the root cause can be conducted and a new hypothesis and countermeasures can be trialed.
Helen DeVos Children’s Hospital iHub Model for Improvement
The Helen DeVos Children’s Hospital (HDVCH) mission is to be the safest children’s hospital in the nation. In order to achieve this vision, staff, providers and hospital leaders continually embrace improvement in order to provide high quality, safe and effective care to our patients and their families while mindfully keeping our workforce safe. Dr. Bob Connors, president of HDVCH, envisioned a model that would support high impact improvement work more quickly and efficiently. This model is termed the iHub.
IHub is a team-based model to rapidly improve the most essential elements of service Spectrum Health provides to patients and families. It is characterized by integrated improvement, engagement of staff and exceptional patient outcomes. Participants in each iHub include a cross-sectional group of clinical and operational leaders from across the system.
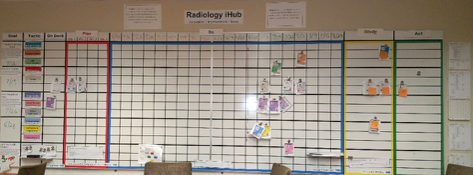
The iHub concept relies upon process improvement principles and tools to support improvement work. Projects begin with a SMART aim statement that aligns to one of five key improvement strategies: (1) people/culture, (2) preventable harm/quality, (3) patient care/experience/access, (4) finance/cost/growth, and (5) systemness/pediatric clinical standardization. All projects use quality improvement tools such as a fishbone diagram or the 5 Whys to understand current and desired state. Projects then proceed through a series of Plan-Do-Study-Act (PDSA) cycles. Each project is managed using an A3 and progress is tracked on a visual management board.
The iHub model overcame previous improvement silos by co-locating quality, safety, simulation, process improvement, human factors and infection prevention specialists in the same physical space so they may collaboratively support improvement work. The majority of improvement project ideas are generated by frontline providers, and the iHub team members (aka Catalyst Team members) support them by coaching and facilitating the work using process improvement principles.
Impact of the HDVCH iHub model includes:
 IHub has fostered high impact improvement work using scientific rigor, quality improvement methods and process improvement tools to support all projects. To date, nearly 40 projects have been completed through the iHub. These projects have engaged nearly 200 direct caregivers and physicians in improvement work at HDVCH.
IHub has fostered high impact improvement work using scientific rigor, quality improvement methods and process improvement tools to support all projects. To date, nearly 40 projects have been completed through the iHub. These projects have engaged nearly 200 direct caregivers and physicians in improvement work at HDVCH.
- Prior to implementation of iHub, it was estimated that 0.40% of HDVCH staff was engaged in improvement work; additionally the number of improvement projects and healthcare disciplines involved in improvement work was uncertain. Since implementation of the iHub, direct caregivers and physicians from 37 healthcare disciplines have been in engaged in improvement work with nearly 3.8% HDVCH staff engagement.
- iHub has achieved notoriety and acclaim not only throughout the Spectrum Health delivery system but nationally by external hospitals and organizations. Other areas of the delivery system have already adopted the iHub model (e.g. Women & Infant Services, Radiology, Surgical Services, Nutrition) while others plan to implement soon. Leaders from other children’s hospitals and healthcare organizations have already visited or plan to visit the iHub space. Additionally, Dr. Connors and members of the Catalyst Team have been invited to speak at local, regional and national conferences about the iHub.
Medication Safety Exemplar Using A3 thinking
 An example of SHGR nursing using the A3 process involved assuring that patient medications were not left in rooms when patients transitioned out of the unit. In the prior state, medications were in a locked drawer in the patient room accessible to nurses using a keyed entry. The problem identified was that these medications were sometimes not returned to pharmacy after a patient left the unit, creating a potential safety issue.
An example of SHGR nursing using the A3 process involved assuring that patient medications were not left in rooms when patients transitioned out of the unit. In the prior state, medications were in a locked drawer in the patient room accessible to nurses using a keyed entry. The problem identified was that these medications were sometimes not returned to pharmacy after a patient left the unit, creating a potential safety issue.
The “Medications in Drawer” team utilized A3 thinking to identify an experiment involving the use of visual management to ensure medications are removed from patients rooms prior to discharge or transfer. This involved a medication box that was visible to individuals in all roles, but accessible only to licensed staff, and transparent to view the contents. This box is intentionally a vibrant orange color to draw awareness. Standard work was developed to include multiple stakeholders to intervene if medications were not removed upon transition. Specifically, it was identified that Environmental Service employees were an integral part of this process, and empowered them to suspending the room cleaning process prior to cleaning if medications were not removed to ensure patient safety.
 A multidisciplinary team experimented with the new process on three different units which included: Butterworth 6 South, Blodgett 3D and Helen DeVos Children’s Hospital 6 CH. Over a three-month period, 31 potential patient exposures to remaining medications were averted through utilization of visual management with the medication boxes. After the experiment, staff verbalized the value the experiment provided. A rollout of visual management medication boxes to all SHGR patient rooms is planned.
A multidisciplinary team experimented with the new process on three different units which included: Butterworth 6 South, Blodgett 3D and Helen DeVos Children’s Hospital 6 CH. Over a three-month period, 31 potential patient exposures to remaining medications were averted through utilization of visual management with the medication boxes. After the experiment, staff verbalized the value the experiment provided. A rollout of visual management medication boxes to all SHGR patient rooms is planned.
