Improving Sepsis Care at Spectrum Health
More than 1.7 million people in the United States (U.S.) are diagnosed with sepsis each year, one every 20 seconds and the incidence is rising 8% every year. Sepsis mortality is high; 270,000 people die from sepsis every year in the U.S., one every 2 minutes; more than from prostate cancer, breast cancer and AIDS combined (Sepsis Alliance, 2018). Sepsis has been identified as a strategic care flow priority for all of Spectrum Health. With a vision to be the national leader for health by 2020, nurses and providers from Helen DeVos Children’s Hospital, Butterworth and Blodgett hospitals recognize that we have an opportunity to improve patient outcomes related to sepsis. Pediatric and adult sepsis teams are focused on early identification, multi-disciplinary communication, and rapid treatment of sepsis through use of evidence-based bundled care. Both teams are early in their work focused on setting the groundwork for standard response and evaluating best practice to assure positive outcomes for patients.
Improving Adult Sepsis Mortality through Early Identification and Rapid Treatment in the SHGR Adult Emergency Departments
At the start of Fiscal Year 2018, the adult Sepsis Mortality rate for SHGR was 32.1 %, exceeding the national benchmark of 16.4%. With the aim to improve this statistic, the sepsis team completed a program assessment and created a timeline of improvement activities to reduce sepsis mortality. Work was started in the Emergency Department because approximately 85% of patients with sepsis meet sepsis criteria on admission to the hospital. The team thought that starting work here would have the largest impact on overall mortality.
Sepsis mortality can be reduced by quickly identifying when a patient has sepsis, and providing rapid treatment. The goal of the sepsis initiative is to reduce sepsis mortality by improving early identification and interventions of sepsis in the emergency department. An assessment of the sepsis response process in the adult Spectrum Health Grand Rapids Emergency Department revealed opportunity to improve the consistency in applying the process in practice. Nurses play a large role in preventing sepsis mortality as they are responsible for administering most of the life-saving treatment measures.
The SHGR Adult (Butterworth and Blodgett hospitals) Emergency Departments (ED) held a multi-disciplinary, 1-day sepsis process improvement event in February 2018. The team identified a need for early identification of sepsis, accelerated treatment, and accountability for outcomes. Action items the team developed included an evidence-based screening tool, process for activating the Sepsis Response, and two separate multi-disciplinary huddles that occur when the patient is first taken to an ED bed and then 90 minutes after the first huddle.
The new screening process starts with the triage nurse. During the triage process, if the patient screens positive for two Systemic Inflammatory Response Syndrome (SIRS) signs, one organ dysfunction sign, and a potential infection, the triage nurse communicates with the bed traffic control nurse or charge nurse to elevate the patient to a “priority 1” acuity (status that trauma, stroke, and STEMIs receive) and pages out the Sepsis Response. Upon receiving the page, the clinical nurse, provider, and pharmacist meet at the patient’s bedside to develop a treatment plan. After the plan has been developed, the clinical nurse, sometimes with assistance from the charge nurse or trauma nurse, draws labs, hangs IV fluid boluses, and administers antibiotics. Approximately 90 minutes after the initial huddle the nurse and provider meet again to reassess the patient, determine if treatment elements have been completed, and discuss next steps in the patient’s care.
Outcomes
The ED Sepsis Orderset is a pre-defined collection of clinical orders including nursing, laboratory and pharmacological interventions based on current clinical evidence to help provide optimal, standardized care for patients seeking emergency treatment of severe sepsis and septic shock. Increased utilization of the ED Sepsis orderset demonstrates adherence to standardized, evidence based care for sepsis patients in the ED. In the first 30 days post go-live, ED Sepsis Orderset utilization increased from 41% to a 48.9%. Subsequently, the Adult Emergency departments have shown continued improvement and sustainment as evidenced by a May order set utilization rate of 68.2%.
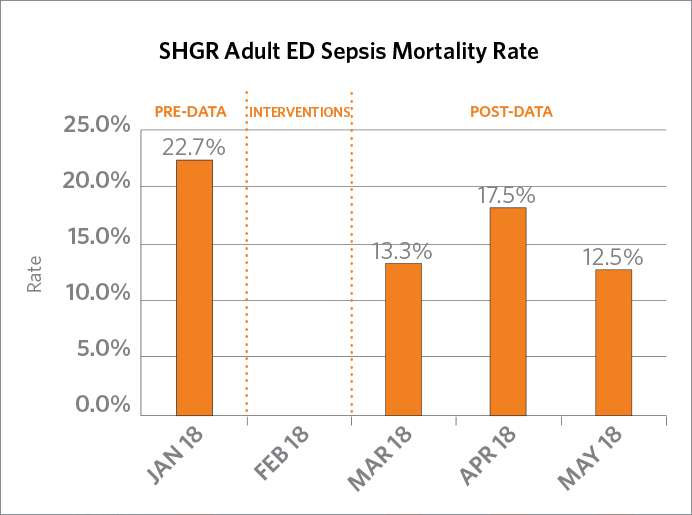
Through the use of Sepsis Response, the Adult Emergency Department Sepsis Mortality rate has decreased from a prior average of 22.7% in January 2018 to 13.3% in March, 17.5% in April, and 12.5% in May 2018.
 |
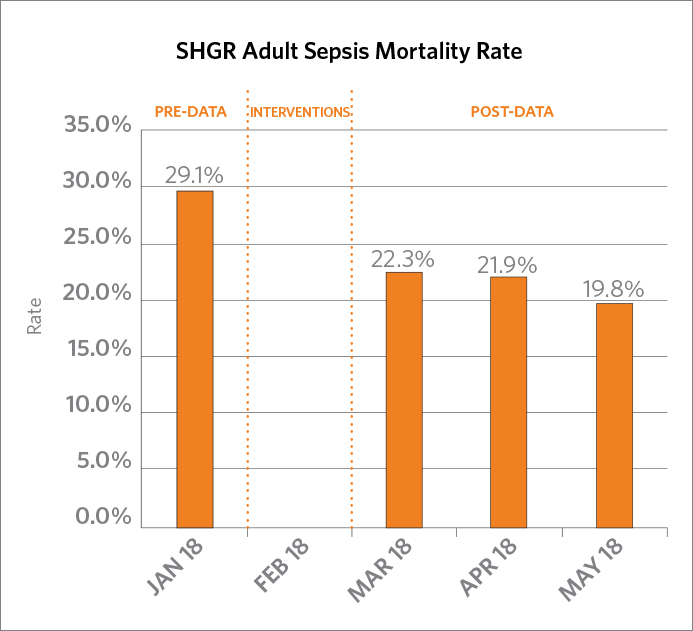 |
Additionally, the early response and treatment efforts in in Adult ED Departments have positively impacted the SHGR Adult Sepsis mortality rate which includes all severe sepsis and septic shock patients at Butterworth and Blodgett hospitals. The average prior to the PI event was 29.1% in January 2018. Post intervention mortality was 22.4% in March, 21.9% in April, and 19.8% in May 2018.
Sepsis Process Improvement Team
Jeff Skinner, MHA, BSN, RN, CEN, Nurse Manager, Butterworth Emergency Department
Stephanie Mullennix, MSN, RN, CEN, Clinical Nurse Specialist, Emergency Department
Tonja Moyer, MBA, SSMBB, BSIE, Improvement Specialist, Senior, Process Improvement
JoAn Beckman, MSN, RN, CCRN, CEN, clinical nurse, Emergency Department
Evan Donnelly, BSN, RN, clinical nurse, Emergency Department
Katie Limbacher, BSN, RN, clinical nurse, CEN Emergency Department
Carla Johnston, BSN, RN, CEN, clinical nurse, 4 Heart Center Intensive Care Unit
Sarah Wright, BSN, RN, clinical nurse, Emergency Department
Brandon Zolynsky, BSN, RN, CEN, Nurse Manager, Blodgett Emergency Department
Melissa Rykse, MSN, RN, CNL, CEN, Supervisor, Blodgett Emergency Department
Kristen Buck, MSN, RN, Sepsis Improvement Specialist, Lead, Acute Health
Sarah Fisher, MSN, RN, CPHQ, Improvement Specialist, Lead, Quality Improvement
Nicholas Kuhl, MD, FACEP
Gregory Kwiatkowski, PharmD, BCPS, Clinical Pharmacy Specialist
Improving Pediatric Sepsis Care at Helen DeVos Children’s Hospital (HDVCH)
In 2016, HDVCH joined the Children’s Hospital Association Improving Pediatric Sepsis Outcomes (CHA IPSO) national collaborative. The goal of the sepsis initiative is to decrease hospital acquired severe sepsis and sepsis mortalities by 75% by the year 2020. The HDVCH hospital acquired severe sepsis rate is 0.02, which is slightly below the CHA collaborative rate.
An initial kick-off meeting to introduce the CHA initiative to a large multidisciplinary group occurred in October of 2016. In January 2017, following guidelines developed by the CHA IPSO national collaborative, HDVCH established a Sepsis Steering Committee and Implementation Teams from each of four care areas: ED; Heme/Onc/BMT (9CH); Medical Surgical (5CH, 6CH, 7CH); and Pediatric Critical Care Unit (PCCU). Each team consists of a physician and Clinical Nurse Specialist (CNS) who serve as co-leads for their area as well as bedside nursing staff clinical nurses and other Interprofessional team members. Each team’s co-leads are also active members of the Sepsis Steering Committee. CHA has determined a best practice bundle which includes seven key drivers/bundle elements.
- Prevention
- Recognition
- Diagnostic evaluation
- Resuscitation/Stabilization
- De-escalation
- Engagement of patients and families
- Optimizing performance
Bundle elements consist of a sepsis screening tool, sepsis huddle, use of a sepsis pathway and sepsis order sets to improve outcomes for the pediatric patient population. Each implementation team met regularly to determine what should be included in the sepsis screening tool and what a sepsis huddle should look like in their area. Appropriate screening tools were trialed in all areas by nursing staff to determine frequency of false positive results. The medical/surgical units and Heme/Onc/BMT care areas collaborated to develop a screening tool that could be utilized in all of the units.
Each team also determined what a sepsis huddle should look like in their areas and utilized simulation to determine the best process. The medical/surgical units and Heme/Onc/BMT team collaborated to develop a non-ICU huddle response. During a sepsis huddle, rapid assessment, communication and determination of appropriate interventions to treat sepsis should occur. Physicians, Nursing, Hospital Supervisors, Residents as well as members from Pharmacy and Lab collaborated on the huddle. Multiple simulations occurred until the team felt the huddle flowed appropriately.
Nursing team members from the PCCU and ED implementation teams also participated in the development of the sepsis pathway and order sets.
The non-ICU and PCCU units began screening patients for sepsis on paper, with plans to screen electronically in the future, the sepsis huddle and use of a pathway on February 28, 2018. The ED implemented screening patients for sepsis electronically, sepsis huddles and use of a pathway on March 22, 2018.
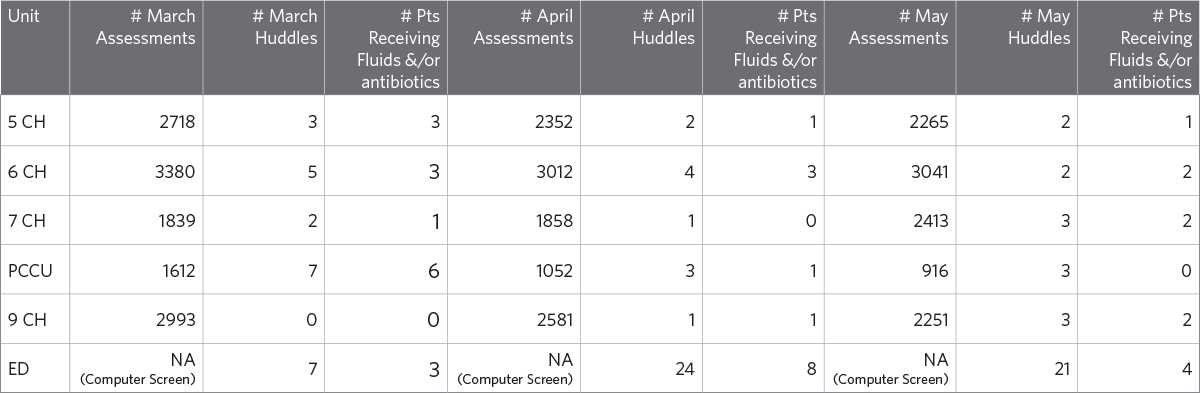
Since implementation of the sepsis bundle elements, HDVCH has had over 90 sepsis huddles and started fluids and antibiotics on more than 35 patients. Our current scope of work is to collect and investigate our process data while we work with IS to develop reports to identify our sepsis patient population and bundle elements. Currently we are impacting at the clinical level with active clinical participation in the screening and huddles processes.
Implementation Teams
ED Team
- Sarah Moultrie, MSN, CPNP-AC, CPEN, Clinical Nurse Specialist, HDVCH ED – no longer with Spectrum Health
- Rachel Clark, MSN, RN, CPNP-PC, Clinical Nurse Specialist, HDVCH ED
- Andrew Peklo, MSN, RN, CEN, Nurse Manger, HDVCH ED
- Heather Blockland, BSN, RN, CPEN, Nurse Educator, HDVCH ED
- Amanda Fleeger, BSN, RN, CPEN, Nursing Supervisor, HDVCH ED
Heme/Onc/BMT Team (9CH)
- Lynn Stachel, MSN, RN, CPON, Clinical Nurse Specialist, Pediatric Heme/Onc/BMT
- Kathy Moore, BSN, RN, CNML, Nurse Manager, 9CH
- Eric Tornga, BSN, RN, clinical nurse and High Reliability Mentor, Pediatric Heme/Onc/BMT
Medical/Surgical Teams (5 CH, 6 CH, 7 CH)
- Ashleigh Kearns, MSN, RN, CPN, Clinical Nurse Specialist, Pediatrics
- Sarah Butterfield, BSN, RN, CPN, clinical nurse, 6CH
- Patti Christensen, ADN, RN, CPN, clinical nurse, 5CH
- Ashley Sorenson, BSN, RN, CPN, clinical nurse, 7CH
- Jamie Dykstra, BSN, RN, CPN, Nurse Manager, 6CH
PCCU Team
- Caryn Steenland, MSN, RN, CCRN, ACCNS-P, Clinical Nurse Specialist, PCCU
- Nikita Vandenbosch, RN, CPNP-AC, Nurse Practitioner, PCCU
- Nicole Leblanc, BSN, RN, CCRN, Nurse Educator, PCCU
- Kayla Miller, BSN, RN, clinical nurse and High Reliability Mentor, PCCU
Other RN Team members
- Susan Teman, BSN, RN, CPPS, HDVCH Senior Improvement Specialist – Safety & Simulation
- Jennifer Krause, BSN, RN, CPN, HDVCH Senior Improvement Specialist – Safety & Simulation
- Amanda Vandenberg, MSN, RN-BC, CNL, CPN, Nurse Educator, HDVCH Staff Development
- Sandy Zuiderveen, BSN, RN, CPHQ, Virtual Pediatric System (VPS) Coordinator
- Jessica McClusky, MSN, RN, CPN, CIC, HDVCH Infection Preventionist
- Nancy Vanhouten, BSN, RN, HDVCH Hospital Supervisor
- JoAnn Mooney, BSN, RN, PCN, CPPS, Senior Improvement Specialist – Quality
